1. Indications:
A: The indications for repairing varicoceles in adolescents include the following:
- Palpable (especially Grade III) left varicocele associated with decreased testicular size (with the volume of the left testis being at least 20% less than that of the right) Palpable (especially Grade III) varicocele with abnormal semen analysis results or
- Large (Grade III) symptomatic (painful) varicocele or
- Bilaterally palpable varicocele with testicular atrophy
Although preventive treatment of adolescent varicocele for the prevention of future infertility and androgen deficiency is controversial, the author feels that it is much easier to prevent future infertility and androgen deficiency than to treat it once it has occurred. In view of the high success rate and low morbidity of microsurgical repair, repair of Grade III varicoceles is the conservative therapy since it conserves testicular function.
B: Based on the Best Practice Policies for Male Infertility of the American Urological Association (AUA) and Society and Society for Reproductive Medicine and Urology (SMRU), varicocele treatment should be offered to the male partner of a couple attempting to conceive when all of the following are present:
- A varicocele is palpable (can be felt);
- The male partner has one or more abnormal semen parameters or sperm function test results;
- The couple has documented infertility;
- The female partner has normal fertility or potentially correctable infertility.
In addition, testicular pain associated with varicocele (in the absence of other pathology), psychological concern regarding future fertility, and cosmetic reasons are all relative indications. Varicocele repair is not indicated in men with normal semen analysis, sperm function assays or only a subclinical (non-palpable) varicocele.
2. Microsurgical inguinal and sub-inguinal varicocelectomies: The preferred approaches:
Subinguinal microsurgical varicocelectomy is currently the most popular approach. It has the advantage of allowing the spermatic cord structures to be pulled up and out of the wound so that the testicular artery, lymphatics and small periarterial veins may be more easily identified. In addition, an inguinal or subinguinal approach allows access to the external spermatic and even gubernacular (scrotal) veins , which may bypass the spermatic cord and result in recurrence if not ligated. Lastly, an inguinal or subinguinal approach allows access to the testis for biopsy or examination of the epididymis for obstruction or repair of hydrocele.
Anesthesia: If the testis is delivered, as described below, regional or light general anesthesia is preferred. If only the cord is delivered, local anesthesia with a 50-50% combination of 0.25% bupivacaine and 1% lidocaine is satisfactory with adjunctive intravenous heavy sedation. After infiltration of the skin and subcutaneous tissues, the cord is infiltrated prior to delivery. Blind cord block carries with it a small risk of inadvertent testicular artery injury. A 30-gauge needle should therefore be employed for cord block to minimize the risk of injury and hematoma.
Inguinal and Subinguinal Approaches:
After standard preparation and draping of the patient, the position of the external inguinal ring is marked as " X" on the skin. The incision extends about 2 cm from the mark following natural skin line . The size of the incision depends somewhat on the obesity of the patient and the size of the testicle being delivered.
The spermatic cord is exposed by hooking an index finger under the external inguinal ring while sliding a small Richardson retractor in the incision along the dorsum of the index finger and pulling in the opposite direction .The cord is encircled with a Babcock clamp. With gentle traction the cord is exposed, encircled with a Babcock clamp, and delivered. The ilioinguinal and genital branches of the genitofemoral nerve are excluded and preserved. The Babcock clamp is replaced with a Penrose drain and the testis is delivered.
The gubernaculum is carefully inspected and any veins encountered are either electrocoagulated or clipped and divided depending on their size. All perforating external spermatic veins and gubernacular veins are also divided. The gubernacular veins have been demonstrated radiographically to account for 10% of varicocele recurrences.

Delivery of the testicle enables the surgeon to identify and ligate these vessels, which are responsible for some varicocele recurrences.
Once all external spermatic perforators and gubernacular veins have been divided, the testicle is returned to the scrotum and the spermatic cord remains elevated over a large Penrose drain for stabilization in preparation for microscopic examination.
The operating microscope is then brought into the operating field and the cord is examined under 8 to 15-power magnification. The internal and external spermatic fascias are opened longitudinally and the cord is examined. The magnification is increased to 15 power and 1 % papaverine is dripped over the cord.
The testicular artery is identified by its pulsation and is dissected free from all surrounding tissue, tiny veins, and lymphatics using a fine-tipped, non-locking micro-needle holder and Pierse tissue forceps. The pulsation of suspected by seeing a pulsating column of blood appears just over the needle holder.
Before beginning the dissection, the cord is inspected under 15 to 20 power magnification for the presence of pulsations, indicating the location of the underlying testicular artery.
The VTI 20 MHz Microvascular Doppler probe is useful in helping to identify the artery, which is often hidden within a network of veins.
The artery is identified and then encircled with a vessel loop to preserve it. Any additional artery encountered are also identified and preserved in this manner.
All remaining internal spermatic veins with the exception of the vasal veins are clipped with hemoclips or ligated and divided. Care is taken to preserve a majority of lymphatics as these can contribute to hydrocele formation postoperatively when divided.
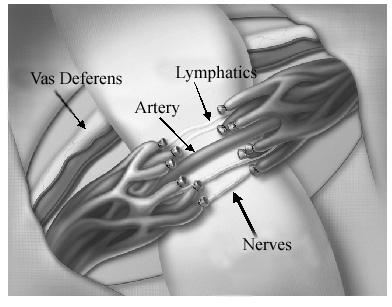
At the completion of varicocelectomy, the cord should contain only the testicular artery or arteries, vas deferens and associated vessels, cremasteric muscle (with its veins ligated and artery preserved), and spermatic cord lymphatics.
This meticulous approach to varicocelectomy requires extensive training and the use of a high-quality operating microscope. Even loupe magnification is inadequate for the reliable identification of the tiny vascular channels and lymphatics of the spermatic cord. The procedure is always performed on an ambulatory basis. Some authors have advocated radiographic percutaneous embolization for isolated left-sided varicoceles and laparoscopy for bilateral varicoceles. Failure rate for radiographic embolization is 15-25% but the late failure rate is much higher. The procedure is not durable. The laparoscopic approach requires general anesthesia, makes presentation of the testicular arteries and lymphatics much more difficult and is associated with great potential morbidity.

