No-Scalpel Incision
A standard vasectomy is performed through one or 2 small scrotal incisions. Once the procedure starts, one may experience mild discomfort when local anesthesia is administered. However, once the anesthesia takes effect one should feel no pain. Some men feel a slight "tugging" sensation as the vasa are manipulated. Following local anesthesia, the vas deferens are isolated on each side and skeletonized of its surrounding tissue, vessels and nerves. Multiple redundant steps are routinely taken in order to ensure discontinuity of the vas deferens and prevent recanalization. These steps can include transection of the vas with removal of an intervening segment, cauterization of the lumen of the vas deferens, ligation of the vas with a clip or suture, and transposition of a tissue layer between the cut ends of the vas.

No-Needle Anesthesia with the MadaJet
Most vasectomies are done right in the doctor's office, or in a clinic. The ideal Vasectomy results in minimal bleeding and almost no intra-operative pain. A vasectomy is facilitated by a warm antiseptic solution for the skin preparation and a warm procedure room (20C to 25C), which allows relaxation of the scrotal dartos muscle, facilitating easy isolation and fixation of the vas deferens.
The patient is placed in a supine position (lying on his back). Surgical preparation includes shaving of the skin of the upper scrotum and retraction of the penis, keeping it out of the way. On average the procedure takes roughly 20-30 minutes.
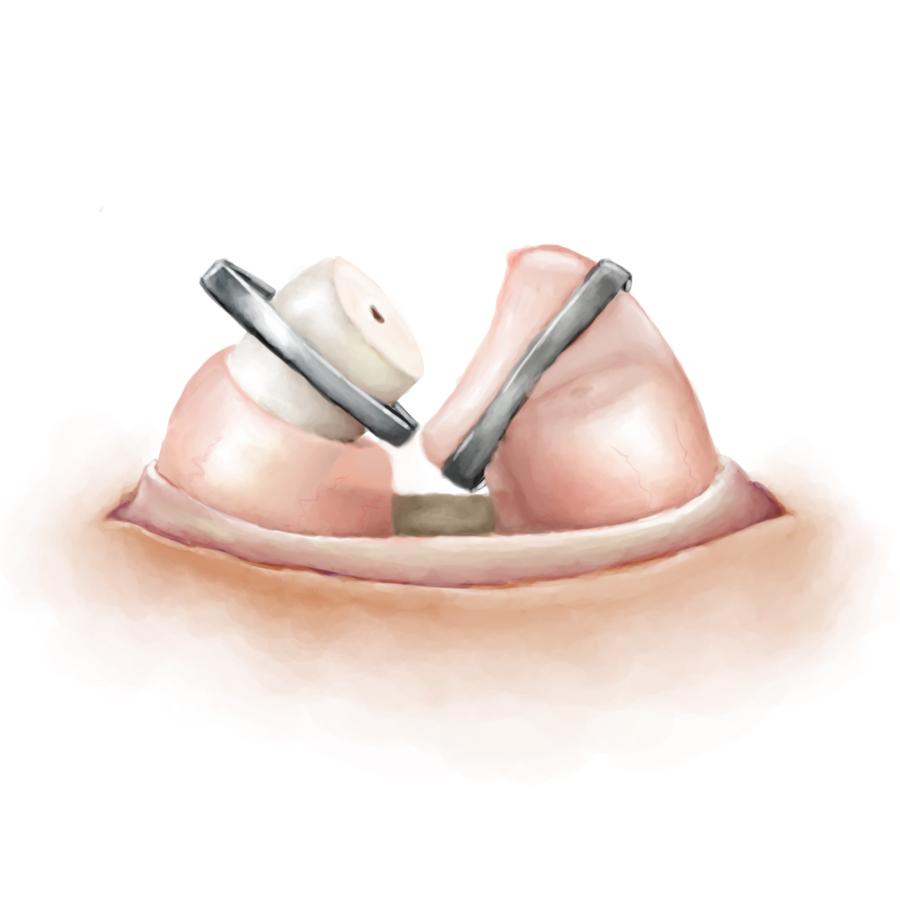
Fascial Interposition
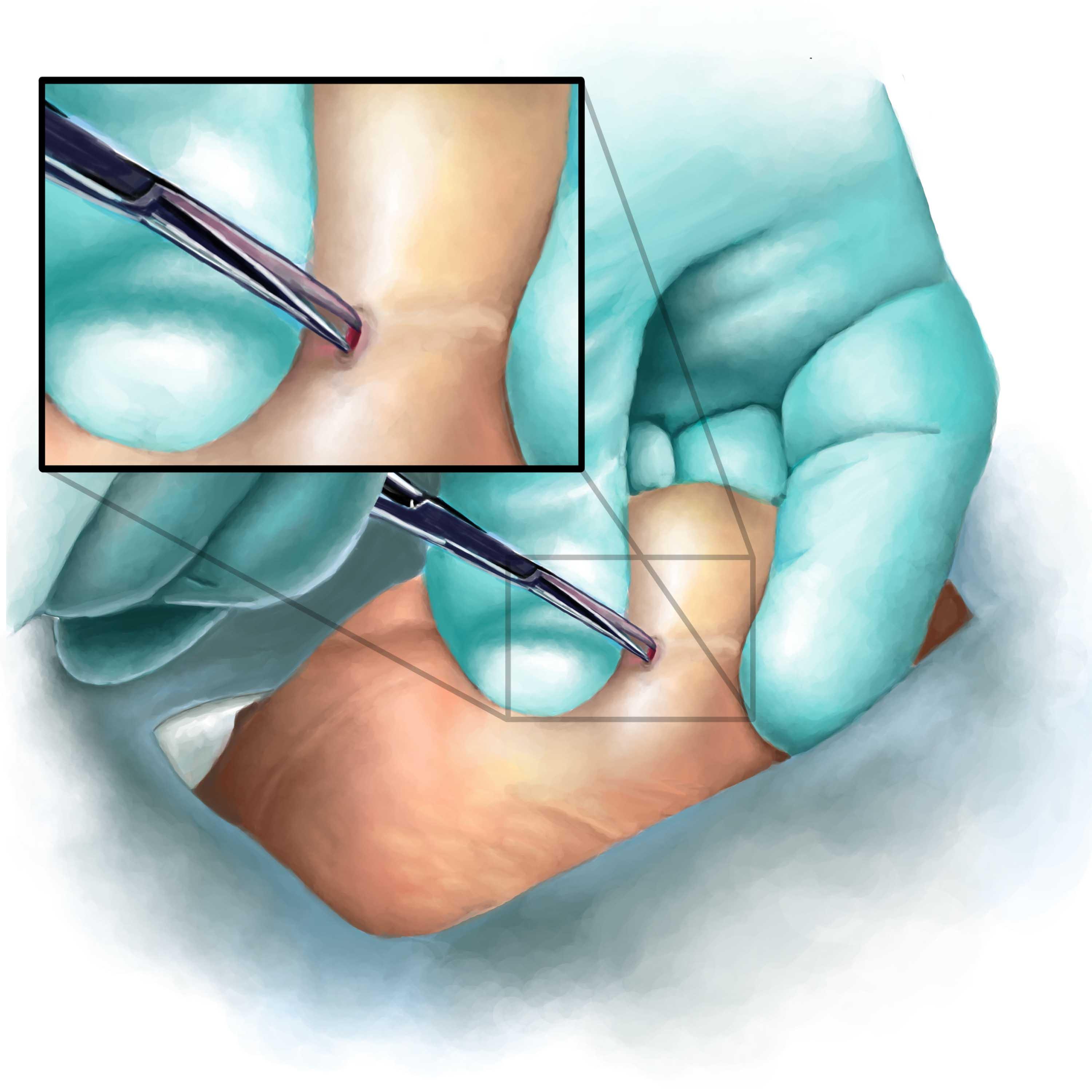
No-Scalpel Vasectomy (NSV)
The No-Scalpel Vasectomy uses an advanced technique to access the vas deferens. Two special instruments are used for this procedure. A scalpel is not needed. These two instruments are (1) ring fixation forceps and (2) dissecting forceps
The benefits of NSV are:
- Fewer complications. It results in almost 10 times fewer hematomas, infections, and other complications—a rate of 0.4% for NSV versus 3.1% for conventional vasectomy.
- Less bleeding and pain.
- Faster and no sutures needed. With hands-on training and practice, NSV can be performed up to 50% faster than the conventional technique.
- Enhanced popularity. Increased patient satisfaction with NSV results in good word of mouth and the enhanced popularity of vasectomy for permanent contraception.
The chance of failure after No-Scalpel Vasectomy at Cornell is about 0.1%. The most frequent complaints after vasectomy are swelling of the scrotal tissue, bruising, and minor pain. While these symptoms generally disappear without treatment, ice packs and scrotal support provides relief. More serious complications of the No-Scalpel Vasectomy, such as hematomas and infection, are uncommon, less than 0.1% at Cornell.
Vasectomy Reversal
An estimated 2% to 6% of men undergoing vasectomy may request a reversal at a later date. In many cases, the cut ends of the vas deferens can be surgically reattached. However, this operation, a microsurgical vasovasostomy, is expensive and, for a variety of reasons, does not guarantee a return to fertility. Vasectomy reversal appears to be more successful if performed within 10 years of the vasectomy, but again, there is no guarantee that fertility will be restored. Vasectomy should therefore be considered a permanent procedure. Before you choose to have a vasectomy, make quite sure that you and your partner do not want any more children. If you are thinking about a reversal now, perhaps you should take more time to decide whether vasectomy is right for you.
Conclusion
Vasectomy is a simple and effective method for providing permanent contraception. A minimally invasive technique, the No-Scalpel Vasectomy, decreases the incidence of complications and have enhanced the popularity of vasectomy as a means of birth control.

