Despite a large number of animal and human studies, the exact mechanism whereby varicoceles cause impaired testicular function remains uncertain. Theories include abnormally high scrotal temperature, hypoxia due to venous stasis, dilution of intratesticular substrates (e.g. testosterone), imbalances of the hypotalamic-pituitary-gonadal axis, and reflux of renal and adrenal metabolites down the spermatic vein. Data exist to both support and refute each of these possibilities. In addition, nitric oxide,reactive oxygen species,and regulators of apoptosis have all recently been implicated in the pathophysiology of varicoceles. It appears that cigarette smoking in the presence of varicocele has a greater adverse effect than either factor alone.
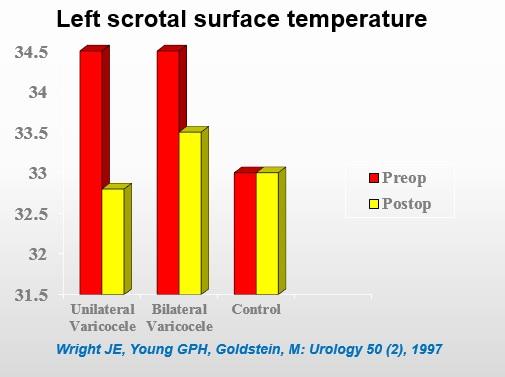
The most vigorously studied pathophysiologic theory is that of increased testicular temperature. It has long been observed that even minor fluctuation in temperature can affect spermatogenesis and sperm function. It has been suggested that varicoceles impair testicular thermoregulation by disrupting the countercurrent heat exchange mechanism in the pampiniform venous plexus. Reversal of testicular blood flow abnormalities and a drop in testicular temperature have been seen in the rat after varicocele repair.18 Recently, Wright and colleagues showed in humans that scrotal skin surface temperatures were elevated in men with varicoceles compared to control patients. Following varicocele ligation, scrotal temperatures returned to a level nearly identical to those of controls. Previous studies have demonstrated that scrotal skin surface temperatures reliably reflect intratesticular temperatures. The pathophysiology of varicocele is probably multi-factorial.