Cryptorchidism is the most common genitourinary abnormality in male infants, affecting up to 6% of newborn infants. A significant concern in cryptorchidism is the potential impact on fertility, as non-scrotal testes are at a higher temperature than is ideal for normal spermatogenesis, which may result in germ cell loss. Even when corrected at an early age, cryptorchidism can result in non-obstructive azoospermia (NOA). Microdissection testicular sperm extraction (TESE) with intracytoplasmic sperm injection (ICSI) has been used successfully to treat men with NOA. We aim to present our updated TESE results in this cohort of men with NOA and a history of cryptorchidism.
Methods
We reviewed a database of 1,882 TESEs performed by a single surgeon (PNS) between 1995 and 2015 and identified 207 cases (11%) in 162 men with a history of cryptorchidism. We analyzed sperm retrieval, fertilization, and pregnancy rates after ICSI. Prior failed attempted procedure (i.e. TESE or biopsy), serum FSH levels, testicle volume, and most advanced testicular histologic pattern were also assessed. Statistics were done using Mann-Whitney u test and chi-square test.
Results
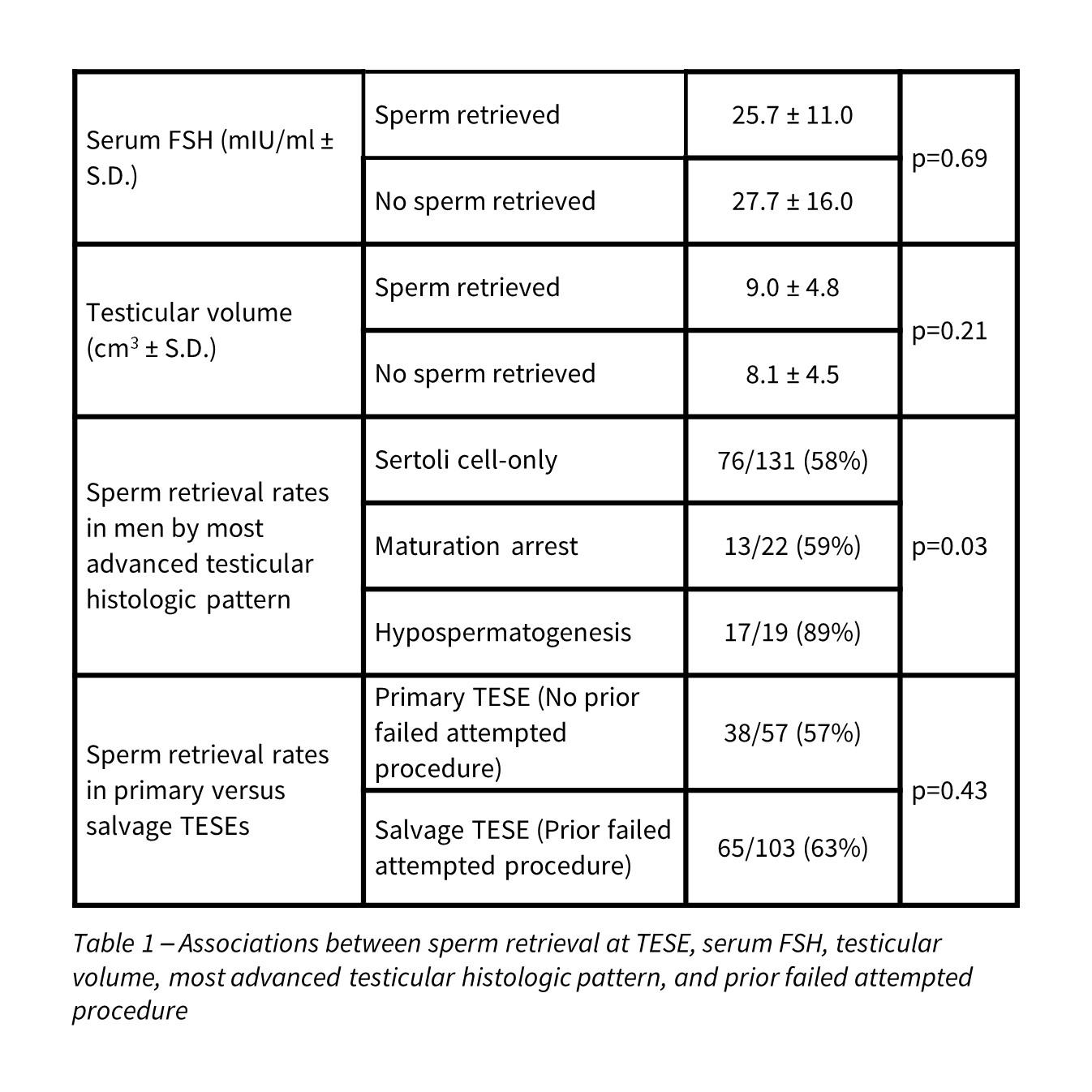
Of the 207 TESEs performed in the cohort of men with a history of cryptorchidism, sperm was successfully retrieved in 128 cases (62%), with fertilization in 713 of 1351 metaphase II oocytes (53%). Of the 128 ICSI cycles where sperm were retrieved, 62 cycles resulted in clinical pregnancy (48%). A most advanced testicular histologic pattern of hypospermatogenesis was a useful predictor of sperm retrieval while prior failed attempted procedure, serum FSH and testicular volume were not useful predictors of sperm retrieval (Table 1).
Conclusions
In this updated review, TESE with ICSI continues to be a successful treatment option for men with NOA and a history of cryptorchidism, with a sperm retrieval rate of 62% and a clinical pregnancy rate of 48%. Sperm retrieval was dependent on most advanced testicular histologic pattern and independent of prior failed attempted procedure, serum FSH, and testicular volume. While our cohort included a large number of men with Sertoli cell-only pattern on testicular histology and men undergoing salvage TESE, which are traditionally difficult populations to treat; both groups demonstrated reassuring sperm retrieval rates of 58% and 63%, respectively.
Date & Time: May 6, 2016 1:00 PM-3:00 PM
Session Title: Infertility: Therapy I
Sources of Funding: This project was supported by The Frederick J. and Theresa Dow Wallace Fund of the New York Community Trust. The project was also supported by grant number T32HS00066 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
- Selected Publication & Abstract

